KCNT1 Epilepsy:
Understanding Current & Emerging Treatment Approaches
An overview of treatment options for families affected by KCNT1-related epilepsy, from current therapies to promising research developments on the horizon.

Treatment Goals & Current Challenges
Primary Treatment Goals
- Reduce seizure frequency and severity
- Improve overall quality of life
- Support developmental progress
- Minimize medication side effects
- Target the root genetic cause when possible
Challenges With Current Approaches
- Unpredictable response to standard treatments
- Significant trial and error process
- Many medications cause sedation
- First year after diagnosis is often most difficult
- Limited disease-modifying options currently available
While conventional treatments provide some relief, they typically address symptoms rather than the underlying genetic mutation. This has driven research toward more targeted approaches that specifically address KCNT1 dysfunction. The ideal treatment would not only control seizures but also support normal brain development and function.
Families often navigate a complex journey of medication adjustments, dietary interventions, and device therapies before finding an effective combination. This process can be emotionally and physically taxing, highlighting the urgent need for more precise treatment options.
Tonic, Focal, or Migrating Seizures
1
Ketogenic Diet
This high-fat, low-carbohydrate diet changes how the brain uses energy, often reducing seizure frequency and severity. It requires strict adherence and medical supervision but has shown effectiveness in many KCNT1 patients.
2
Anti-Seizure Medications
Commonly prescribed medications include Keppra (levetiracetam), phenobarbital, Onfi (clobazam), and Topamax (topiramate). While helpful for seizure reduction, none specifically target the KCNT1 channel dysfunction.
3
Vagus Nerve Stimulation
This implanted device sends regular, mild electrical pulses to the brain via the vagus nerve. VNS can reduce seizure frequency and intensity over time, providing an additional option when medications alone aren’t sufficient.
4
Rescue Medications
Emergency interventions like Diastat (diazepam) and nasal/oral benzodiazepines to stop prolonged or cluster seizures.
5
Infantile Spasms
Used often for infantile spasms, which can occur in some KCNT1 cases, by increasing GABA levels in the brain.
6
Surgical Options
In rare cases, brain resection surgery may be considered when seizures come from one area and do not migrate. However, this is often not a viable option for KCNT1 epilepsy.
Small Molecules & Other Network-Targeting Drugs
These drugs aim to modulate neuronal networks and ion channels, offering various avenues to reduce seizure activity in KCNT1 epilepsy patients. They are crucial for symptom management while targeted gene therapies are still in development.
Repurposed Small Molecules
Existing medications with other primary uses that may help regulate KCNT1 channel activity:
- Carvedilol (originally a heart medication)
- Quinidine (an antiarrhythmic drug)
- Some ADHD and antidepressent medications that affect ion channels
Existing medications are being explored for their potential to reduce KCNT1 channel overactivity. These are often identified through screening approved drugs for new therapeutic applications in epilepsy.
Precision Small Molecules
These lab-designed compounds specifically tailored to address KCNT1 dysfunction:
- Custom channel blockers targeting the specific KCNT1 mutation
- Compounds that modify how the abnormal channel operates
- Medications designed to normalize downstream effects
These are the preferred approach when possible because they are custom-built to directly address the unique KCNT1 channel dysfunction. Although still in early research stages, they offer the potential for more precise seizure control with fewer side effects compared to broader-acting drugs.
Non-KCNT1 Anti-Seizure Drugs
Many conventional and emerging anti-seizure medications work by influencing other ion channels (e.g., sodium, calcium, serotonin receptors) or broader neural networks. These broad-spectrum approaches could provide significant relief while specific KCNT1 solutions are developed. See our section on clinical trials for more information.
RNA & Gene-Targeted Therapies: Addressing the Genetic Cause

RNA-Targeted Therapies
Antisense oligonucleotides (ASOs) and double-stranded interfering RNA (di-siRNA) therapies aim to reduce the faulty KCNT1 message at the RNA level before the protein is made.
They are delivered into the spinal fluid and need repeat doses every few months.
They do not change the gene itself.
Gene Therapy
Gene therapy delivers new genetic instructions into brain cells using carriers like viral vectors or lipid nanoparticles (LNPs).
Different strategies are being explored, including reducing the effect of the mutated gene or adding healthy KCNT1 instructions—though it’s not yet known whether adding WT will help.
LNP-based therapies can be redosed; viral vectors are usually one-time.
Gene Editing
Gene editing uses tools like CRISPR to permanently correct the KCNT1 mutation directly in a cell’s DNA. To work, these molecular “scissors” must be delivered into brain cells using carriers similar to those being developed for gene therapy—such as lipid nanoparticles (LNPs) or other delivery systems capable of crossing the blood–brain barrier (BBB).While still in early research phases, gene editing holds the potential for a one-time, lasting correction of the genetic defect, rather than ongoing suppression.
“Gene-targeted approaches represent a paradigm shift from treating symptoms to addressing the root cause of KCNT1 epilepsy. While challenges remain, these technologies offer unprecedented hope for meaningful disease modification.”
RNA & Gene-Targeted Therapies: Addressing the Genetic Cause
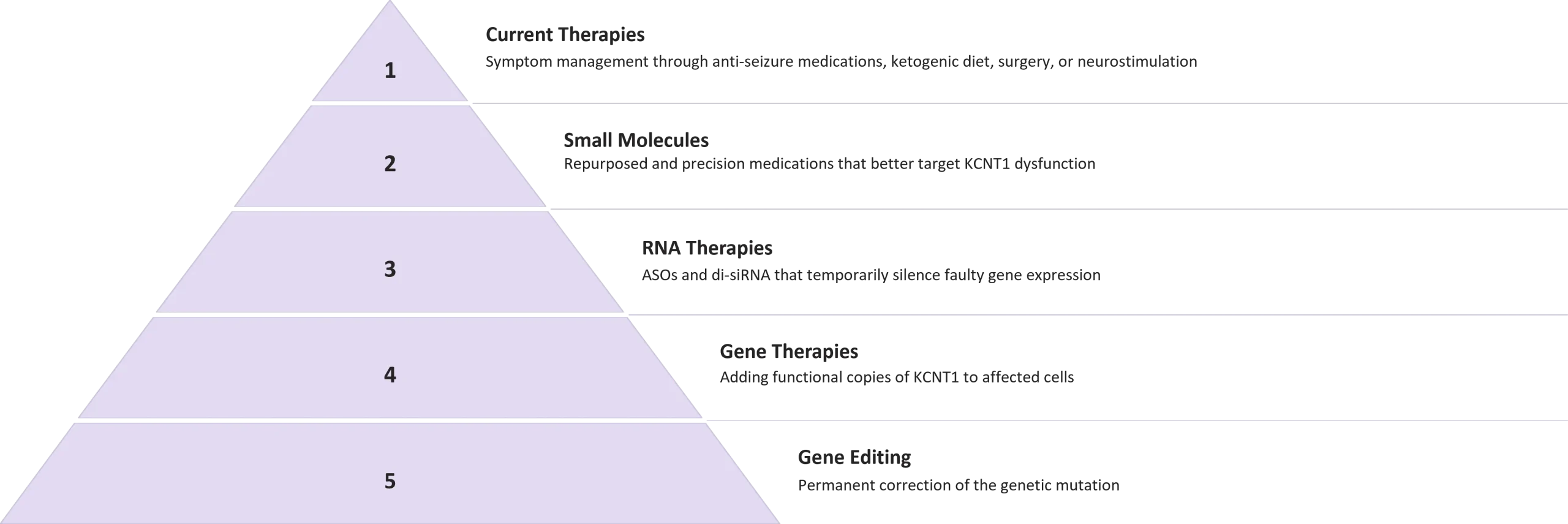
Each advancement in KCNT1 treatment builds upon previous approaches, moving us closer to truly disease-modifying therapies. While current treatments manage symptoms, emerging genetic approaches aim to correct the underlying cause.
Families affected by KCNT1 epilepsy should work closely with their medical team to stay informed about clinical trials and research developments. Treatment plans should be regularly reviewed as new options become available.



