Early-Onset KCNT1 Epilepsies
KCNT1-related epilepsy includes a broad spectrum of conditions, from mild symptoms to severe early-onset epilepsies with drug-resistant seizures and profound developmental delays.
Early-Onset KCNT1 related Epilepsies
Most early-onset forms of KCNT1-related epilepsy begin in the first few weeks or months of life. These children often experience seizures that are frequent, drug-resistant, and significantly impact development. In some cases, seizures begin in the neonatal period or shortly after NICU discharge. Diagnoses often include EIMFS, EOEE, or IS. An electroencephalogram (EEG) is typically needed to help confirm the diagnosis, characterize seizure patterns, and guide treatment decisions.
Epilepsy of Infancy with Migrating Focal Seizures (EIMFS)
- Onset: Typically under 6 months of age; average ~2 months
- Seizures: Focal seizures that move from one side of the brain to the other (“migrating”), often presenting as rhythmic jerking in the face, hands, or feet. Read more on our Seizures page.
- Frequency: Dozens to hundreds of seizures per day
- Often misdiagnosed or not recognized early on
- EEG: Seizures occurring independently in both hemispheres, sometimes with suppression bursts
- Developmental Impact: Profound developmental delays are common
Early-Onset Epileptic Encephalopathy (EOEE)
Seizure Types
Tonic seizures, spasms, myoclonic movements, or generalized seizures
EEG Findings
Diffuse slowing, suppression burst patterns, or multifocal spikes
Disease Course
Seizures may be briefly controlled but often become intractable. Read more on our seizures page.
Development
Developmental regression is frequent following seizure onset
Diagnosis
This category is often used early in diagnosis, before a more specific syndrome is identified

Infantile Spasm Syndrome / West Syndrome
- Onset: Usually between 3–7 months of age
- Seizures: Clusters of sudden flexion or extension movements (e.g., head drops, arm flinging)
- EEG: Hypsarrhythmia (a chaotic, high-amplitude pattern)
- Development: Regression or plateau of milestones around onset of spasms
- Treatment: ACTH and vigabatrin are first-line therapies, but response in KCNT1 related cases may vary
- Evolution: Some children with IS may later be diagnosed with EIMFS or other DEEs
Treatment Options & Medications
There is no cure for KCNT1-related epilepsy yet, but several treatment strategies may help reduce seizure frequency or improve comfort. These can include:
Anti-seizure medications
Most children will try multiple medications. Some may see temporary seizure relief, but many do not achieve full control.
Supportive care
Therapy services, palliative care, and specialized equipment can all improve quality of life.
Ketogenic diet
A high-fat, low-carbohydrate diet that has helped some families reduce seizure frequency.
Clinical trials
Experimental therapies may be available. Families are encouraged to learn more through our Research & Trials page.
Precision Medicine & Investigational Treatments
New targeted therapies are in development for KCNT1-related epilepsy:

Antisense Oligonucleotides (ASOs)
Targets mRNA to reduce the amount of abnormal KCNT1 protein.

Small Molecule Inhibitors
Help restore normal function of overactive KCNT1 channels.

siRNA Therapies
Targets mRNA to reduce the amount of abnormal KCNT1 protein.

Genetic Medicine Approaches
Cell and genetic medicine approaches aim to replace or repair defective genes.
These options are not yet widely available, but several are approaching clinical trial readiness.
Managing Comorbidities in KCNT1 Epilepsy
KCNT1-related epilepsy is often accompanied by comorbidities requiring specialized care:
Balancing Development & Medication
While treatments focus on seizure control, it is equally important to support a child’s physical and cognitive development. Many children with KCNT1-related epilepsy experience significant developmental delays due to seizures and the effects of medications. Caregivers emphasize the importance of balancing seizure control with maintaining development and suggest that parents discuss that the medications used are not overly sedating, as this can further hinder developmental progress.
- Physiotherapy and Regular Therapeutic Support: Physical therapy (PT) and occupational therapy (OT) help children build and maintain motor skills, muscle strength, and coordination. Early intervention improves outcomes and supports weight-bearing to promote bone health and prevent complications.
- Speech Therapy: Supports feeding and communication challenges.
- Minimizing Sedating Medications: Anti-seizure medications can impact alertness and engagement. Monitor side effects and adjust doses to balance seizure control with developmental benefits.

Bone Health and Hip Dysplasia
Patients with KCNT1 epilepsy are at risk for bone problems due to long-term use of seizure medications and reduced mobility. Monitoring bone density and supplementing calcium and vitamin D is crucial. Some medications can affect calcium and vitamin D levels, leading to osteopenia or osteoporosis, increasing the risk of fractures. In addition, children who are unable to walk are at higher risk for developing hip dysplasia, a condition where the hip joint does not develop properly. Over time, this can lead to pain, stiffness, and decreased mobility. In severe cases, hip dysplasia may require surgical intervention to correct the joint alignment and prevent further complications. Regular monitoring of bone density and hip development is crucial, and early intervention with physical therapy or surgery can help manage these complications.
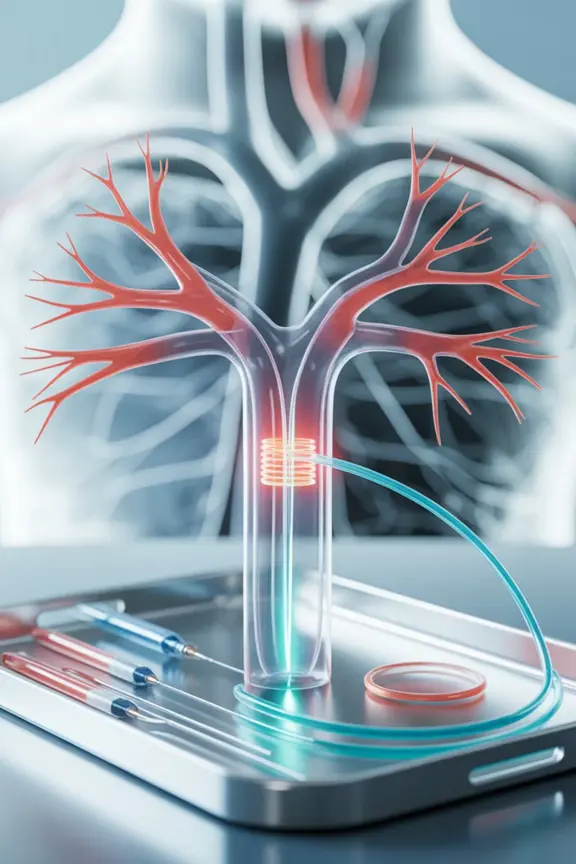
Cardiac or Vascular Issues
A small percentage of patients may have systemic-to-pulmonary collaterals or arrhythmias. An echocardiogram is recommended early on, and a CT angiogram may be needed if collateral arteries are suspected.
Some patients with KCNT1 mutations experience heart or lung problems, including arrhythmias and systemic-to-pulmonary collaterals. These collateral arteries are extra blood vessels that form a connection between the aorta (the main artery from the heart) and the pulmonary arteries (which carry blood to the lungs). Doctors recommends that all children with KCNT1 epilepsy receive an initial cardiology evaluation to check for these conditions. Many doctors suggest that if everything looks good at that first visit, regular cardiology follow-ups aren’t usually needed. However, recent reports from parents show that echocardiograms may not initially pick up the development of any collaterals, and bleeding from the nose or mouth can indicate the presence of collateral arteries and require emergency treatment.
Read our publication in Pediatric Cardiology.
Echocardiogram
This is the main test used to check for collateral arteries.
CT Angiogram
Sometimes, the echocardiogram might miss collateral arteries. If there are other signs or symptoms, a CT angiogram might be needed as it can detect collateral arteries more accurately.
Prevalence
In individuals with KCNT1-related epilepsy, collateral arteries are an uncommon heart-related finding, but research by the KCNT1 Epilepsy Foundation sees heart or lung related concerns in about 10% of patients.
Severity
These vessels can become very extensive, sometimes forming hundreds of tiny blood vessels. These are commonly seen in pulmonary arterial hypertension, fibrotic lung diseases, and inflammatory lung disease.
Symptoms
Collateral arteries can lead to heart problems, such as heart failure or a heart murmur, which can be seen on an ultrasound of the heart (echocardiogram). More severe symptoms include severe bleeding from the lungs (called hemoptysis), which can be very dangerous and even life-threatening.
Current Treatment Options for Systemic-to-Pulmonary Arteries
Coil Embolization
This is a common treatment where doctors try to block off the extra vessels. However, the treatment doesn’t always provide a permanent solution, as the vessels may grow back, resulting in a return of symptoms.
Lobectomy
If the collateral arteries are only in one part of the lung, in rare or extreme cases, removing that part of the lung might be considered.
Medications
Some medicines can help reduce the risk of bleeding, but we’re still learning which ones work best.
Feeding and Swallowing Problems
Many children with KCNT1-related epilepsy have neurological differences that can cause a weak swallow and increase the risk of food or liquid “going down the wrong way” (aspiration). This can also make it harder to give medicines safely and consistently.
Some patients start with partial tube feeding while still eating by mouth, but as the condition progresses, many transition to full tube feeding to make sure they get enough calories, hydration, and safe medication delivery.
To make feeding safer and reduce reflux, certain tube types or additional procedures may help. Some doctors, including Dr. Bearden, recommend avoiding a G-tube by itself if there’s a high risk for reflux, because G-tubes alone can sometimes make reflux worse. Instead, they may suggest:
- GJ-tube feeding, which sends food past the stomach into the small intestine
- A G-tube plus Nissen fundoplication, a surgery that strengthens the valve between the esophagus and stomach to prevent reflux
“While the idea of a feeding tube can feel scary at first, it often improves quality of life—helping children get the nutrition they need and making medicines easier to give,” Dr. Bearden explains.
- Combination of Feeding and Tube Support: Some patients may begin with partial tube feeding while still consuming food orally, but as their condition progresses, many transition to complete tube feeding to ensure they receive adequate nutrition and to safely administer medications.
- Surgical Adjustments Over Time: Feeding needs can change. Gastrointestinal issues such as worsening reflux may require surgical revisions or tube changes over time. In these situations, doctors may recommend switching to a GJ-tube or adding a fundoplication to improve feeding safety and comfort.
- References [add link]
Get more tips from parents on our Symptoms and Treatments page.
Safe Sleep & Home Environment
Ensuring a safe sleeping environment is essential:
- Consider seizure-safe beds and pillows.
- Consider installing padding and monitoring devices (e.g., motion alarms).
Prevent injury during nighttime seizures and support better sleep quality for both child and caregivers.
If you have difficulty obtaining a video monitor, contact us, we may be able to help.

Care Team and Long-Term Support
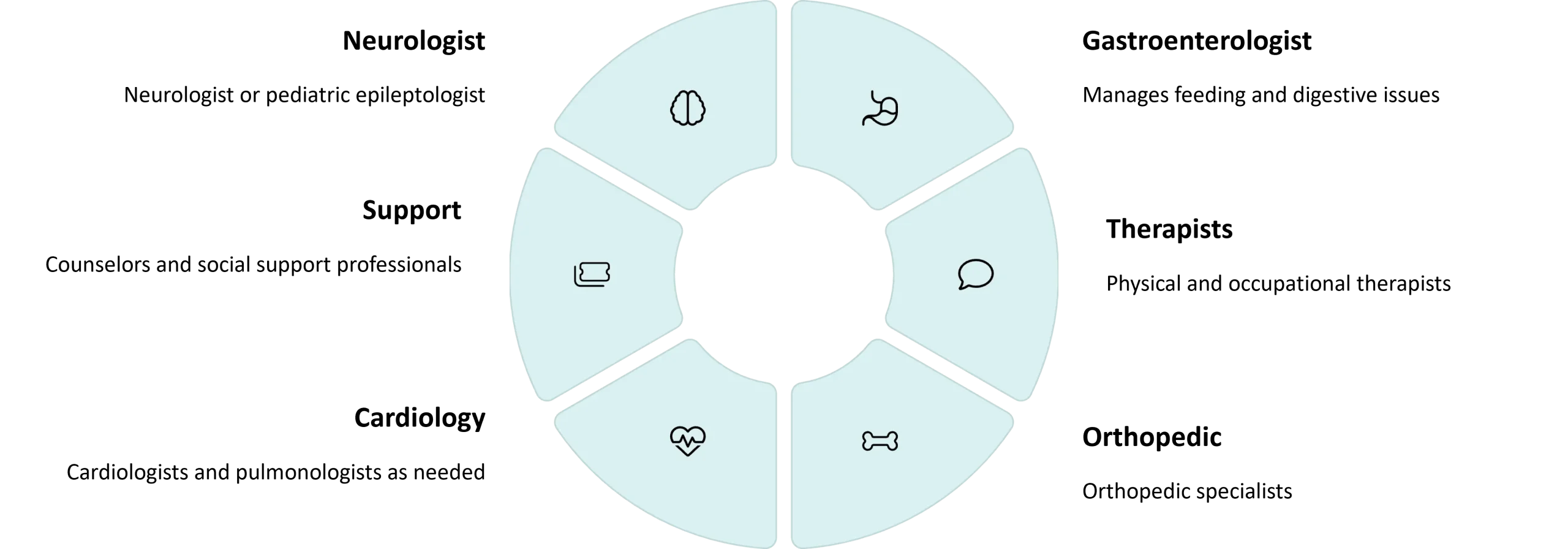
When selecting a neurologist, parents emphasize open communication and availability over KCNT1 expertise.
Understanding Mortality Risk
Families facing early-onset KCNT1 epilepsy often have questions about life expectancy. The reality is that KCNT1-related conditions can carry serious risks, especially when seizures begin very early and are not well controlled. These risks may include:
- Seizures that interfere with breathing or feeding
- Respiratory infections and other medical complications
- Sudden unexpected death in epilepsy (SUDEP)
It’s important to work closely with your care team to monitor health and discuss safety measures, including sleep safety, airway support, and seizure rescue plans. Our Foundation is committed to supporting families across this journey.
If you have lost a loved one to complications from KCNT1, please consider participating in our special mortality study by reaching out.
Participating in Studies, Clinical Trials and the Registry
Families are encouraged to participate in the KCNT1 International Registry—even if symptoms are mild or seizures are absent. This helps researchers understand the full spectrum, including prevalence and penetrance. Stay informed about clinical trial opportunities through the Foundation’s updates.
Your participation may help accelerate the development of more effective, targeted treatments.



